
Aikaterini Psillaki1, Paraskevi Theofilou1*
1Hellenic Open University, School of Social Sciences, Patra, Greece
*Corresponding author: Paraskevi Theofilou, 1Hellenic Open University, School of Social Sciences, Patra, Greece.
Received date: June 17, 2023
Accepted date: June 20, 2023
published date: July 04, 2023
Citation: Aikaterini Psillak, Paraskevi Theofilou. (2023) “Efficacy for appropriate medication use and quality of life in chronic disease patients: The association with duration of treatment and polypharmacy”. International Journal of Epidemiology And Public Health Research, 3(2). DOI: http;//doi.org/04.2023/1.1046.
Copyright: © 2023 Paraskevi Theofilou. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The aim of the present research was to investigate the quality of life and the compliance in taking pharmaceutical preparations in chronic patients over 60 years of primary care. The investigation also included the important parameter of polypharmacy. The research was conducted on chronic primary care patients, over 60 years of age, who live in the wider area of Rhodes. Assessment of quality of life in patients with chronic diseases receiving medication was performed using the Missoula–VITAS Quality of Life Index (MVQOLI). The assessment of the level of compliance with the therapeutic treatment in the patients who participated in the research was carried out using the "Self-Efficacy for Appropriate Medication Use Scale (SEAMS). Statistically significant associations and differences were found between some important dimensions of quality of life, such as well-being or functioning, with adherence and other clinical factors. Adherence to treatment and patient quality of life is a multifaceted phenomenon influenced by many factors related to the patient, health care system, condition, treatment, and socioeconomic background, which interact with each other in many ways.
Introduction
Adherence is defined, according to the WHO, as "the degree to which a person's behavior regarding taking medication, diet or required lifestyle changes coincides with medical instructions" (1). In English terminology, "compliance" is rendered as "adherence" or "compliance", definitions that are considered almost synonymous by professionals, while most use the definition of the World Health Organization to describe them. However, the term "compliance" refers to a passive behavior in which the patient follows a list of instructions from the treating physician, while "adherence" refers to a more positive, proactive behavior that leads to radical lifestyle change from the patient, who must follow a daily regimen or plan agreed with his physician (2). The rate of successful adherence to pharmacotherapy ranges from 15–93% (3) and is a function of the individual's personality, general condition, type of medication, patient-physician relationship, and other socioeconomic parameters. In order for the therapeutic plan to have the desired benefits of the administered treatment, it is necessary that the patients agree with the treating physician and faithfully follow the instructions given to them, otherwise even the "best" therapeutic approach may not have the expected results results (3).
The main determinants of the patient's adherence to the treatment plan range in five main axes according to the WHO and include socioeconomic factors of the patient but also related to his disease, factors related to the type of treatment provided and finally factors related to the professional team health system, the wider health system, the patient and the supportive environment and the relationship that has developed between them. In particular, age, educational level, type of disease, understanding of the benefit of receiving a treatment, complexity of treatment regimen and instructions, possible side effects, cost of treatment, and possible cultural prejudices of the patient regarding the disease and/or treatment play a primary role in following a treatment plan. Another critical factor in adherence is the quality of the relationship with the medical staff. A possible lack of communication between doctor and patient can have an extremely negative impact on compliance. Finally, certain adverse effects and side effects of drugs, which may occur during treatment, such as weight gain, feeling weak, episodes of hypoglycaemia or hypotension can in turn affect the degree of compliance (4-6).
The term polypharmacy was used a century and a half ago to refer to issues related to multiple and excessive drug consumption. It mainly concerns elderly people with chronic multiple morbidities. Since then, it has evolved with different meanings, including but not limited to unnecessary drug use and off-label drug use. Based on our review of current data, the use of 5 or more drugs is an accepted definition of polypharmacy worldwide. This cut-off point of 5 drugs is associated with the risk of adverse outcomes such as falls, frailty, disability and mortality, especially in the elderly population due to their frailty (7). The WHO suggests that, while the definition is numerical, it is important to place particular emphasis on evidence-based practice in prescribing new medicines with the aim of reducing the inappropriate use of multiple medicines. The management of polypharmacy is therefore a challenge for all health care providers worldwide, with the aim of better patient compliance of necessary pharmaceuticals with efficiency, reducing polypharmacy and strengthening skills for rational use of medicines (8).
Although one would expect that improved medication adherence would have a positive impact on quality of life, findings in the literature are not always consistent. A number of studies have identified a positive relationship between medication adherence, quality of life and improved patient-centred treatment outcomes following medication adherence interventions (9-13). However, other studies have not reached the same conclusion of a positive association (14-16). One reason for these inconsistent findings may be the different study populations, settings and tools used to measure quality of life and adherence (9). Finally, in the literature, a gap appears in the association of adherence to treatment and quality of life of elderly patients with chronic diseases, in general, taking into account the polypharmacy factor.
The aim of the present research was to investigate the quality of life and the compliance in taking pharmaceutical preparations in chronic patients over 60 years of primary care. The investigation also included the important parameter of polypharmacy, with the separation of patients into two subgroups, that of patients who take less than five different pharmaceutical preparations daily and that of patients who take five or more different pharmaceutical preparations daily.
Method
Research design
To implement the purpose of this work, a quantitative cross-sectional survey was designed using questionnaires weighted to the Greek population. The variables used to investigate possibly statically significant associations were overall quality of life, the five dimensions of quality of life, which are symptoms, functioning, interpersonal relationships, well-being and spirituality, overall adherence to chronic medication , socio-demographic factors, such as age, sex, educational level, occupation and marital status, but also clinical factors, such as the amount of different pharmaceuticals in tablets per day (<5 or ≥5) and duration of medication in years. For participation in the research, the age limit of 60 years was set based on the definition of elderly people by the WHO, while the limit of ingested tablets, not different substances, per day (<5 or ≥5) was set based on the definition of polypharmacy in most studies from the literature review (7,17).
Sample
The research was conducted on chronic primary care patients, over 60 years of age, who live in the wider area of Rhodes. The selection criteria for participation in the research included the age of 60 years or older, diagnosed with chronic diseases for which they receive at least one pharmaceutical preparation on a daily basis, the ability to communicate in Greek and the satisfactory level of cooperation and understanding. The research population was a convenience sample and included the 65 patients who participated and answered two different questionnaires translated and weighted in the Greek language, namely the quality of life (MISSOULA - VITAS® QUALITY OF LIFE INDEX, VERSION – 15R) and compliance in receiving medication use (Self-Efficacy for Appropriate Medication Use Scale (SEAMS) and completed socio-demographic and clinical data.
Psychometric tools
Assessment of quality of life in patients with chronic diseases receiving medication was performed using the Missoula–VITAS Quality of Life Index (MVQOLI), an instrument created by Byock and Merriman in 1998 to assess individual experience of quality of life of people with advanced disease. Maintaining optimal quality of life is a key objective for palliative care and institutionalized living and therefore the information gathered through the MVQOLI questionnaire assisted in better healthcare delivery by healthcare professionals and early detection and eventual treatment concerns of patients that affected their quality of life (18). Ultimately the MVQOLI questionnaire was adapted and used in many different settings of people with chronic diseases assessing their quality of life while also setting health care delivery, in institutions, in the hospital, at home, in long-term care including assisted living, and in outpatient settings (19). The MVQOLI questionnaire assesses patients' overall quality of life in five individual dimensions, namely symptoms, functioning, interpersonal relationships, well-being, and spirituality. The MVQOLI instrument was specifically designed to assess patients' personal perception or experience of each of these five dimensions. From each dimension, which constitutes a separate area of the overall quality of life, three types of information are collected from the respondents, which include evaluation, i.e., a subjective measurement of the actual situation or circumstance, satisfaction, i.e., the degree of acceptance or knowledge of the actual situation and importance, i.e., the degree to which each dimension has an impact on the same dimension. The main purpose of this tool is the rapid interpretation and use of information on the subjective view of patients' quality of life by health professionals (20,21).
The assessment of the level of compliance with the therapeutic treatment in the patients who participated in the research was carried out using the "Self-Efficacy for Appropriate Medication Use Scale (SEAMS)" questionnaire. The SEAMS tool is a validated self-report scale, based on Bandura's social cognitive theory and subsequently developed for patients with chronic diseases, that measures the patient's confidence in their ability to take their daily medication correctly. The scale has been shown to exhibit high internal reliability and strong validity. It consists of a total of 16 questions, on a Likert scale (1=not at all sure, 2=somewhat sure, 3=very sure) with a possible range of the total rating between 16 and 48. Higher scores indicate better patient self-efficacy in complying with treatment (22). The SEAMS scale was translated from the source language, English, into the target language, Greek, as the Self-Efficacy Scale for Appropriate Medication Use. Translation was completed as outlined in guidelines for adapting instruments to multiple languages and cultures (23). Translators knowledgeable in both the source and target languages and skilled in cross-cultural adaptation of the scale made two independent translations into Greek and two independent translations back into English. The final version was independently reviewed and translated by a bilingual health psychologist without having previously seen the original SEAMS. The back translation was in very close agreement with the SEAMS original, as verified by a professional linguist fluent in both English and Greek. A healthcare professional who knew both languages performed the final language normalization step. This involved editing the target language version of the scale in a consistent way of writing and helped to ensure that patients could easily understand the modified SEAMS version in Greek. Finally, a social expert reviewed the final instrument to check for omissions (24). Next, semantic validity was conducted, which helped to verify the understanding of individual SEAMS items by interviewing the volunteer participants. This stage aimed to identify problems related to the acceptance and understanding of the terms by the research participants. For this stage of the cultural adaptation process, 10 patients with end-stage renal disease answered the SEAMS as well as general assessment questions of the scale, indicating very satisfactory results (24).
In addition to the two separate questionnaires, socio-demographic and clinical characteristics of the patients were recorded, such as age, sex, educational level, profession and marital status, as well as the amount of different pharmaceutical preparations per day (<5 or ≥5) and the duration receiving medication in years.
Procedure
The data was collected by completing the questionnaires in paper form from patients of primary health care facilities (PHC) in the wider area of Rhodes, during the period of March 2023 and April 2023, after receiving the relevant permission from the managers of these facilities. Also, the corresponding approval for the use of the Greek versions of the MVQOLI and SEAMS questionnaires was obtained from the researchers who did the translation and cultural adaptation into the Greek language. The sample was convenience and the collection was performed prospectively, that is, it included patients 60 years of age or older, with chronic diseases, who received at least one pharmaceutical preparation per day and visited primary health care structures during the specific time period. The participants were adults, proficient in the Greek language who had fully understood and signed a consent form for participation in this research. The survey was anonymous and participation was voluntary. All patients were informed about the purpose of the research, their rights, and the possibility to refuse or stop participating in the present study at any time without penalty. All responses and data collected from the questionnaires constituted confidential data used for the purposes of this research.
Statistical analysis
The statistical analysis aimed to investigate possibly statically significant correlations and differences between the main variables resulting from the collection of questionnaire data, such as overall quality of life, the five dimensions of quality of life, which are symptoms, functioning, interpersonal relationships, well-being and spirituality, overall adherence to chronic medication as well as clinical factors. The clinical variable was the number of different medications taken in tablets per day (<5 or ≥5), based on the definition of polypharmacy in most studies from the literature review (7,17).
All statistical analyzes were performed with the Statistical Package for the Social Sciences (SPSS 26.0 for Windows). In the total sample, 65 participants, all questionnaires and questions were answered. A p-value equal to or less than 0.05 was considered to indicate statistical significance. A Kolmogorov-Smirnov test was then carried out to check whether the values of the main variables of the questionnaires, on the basis of which the correlations were then made, in the whole sample fell into a normal distribution.
Results
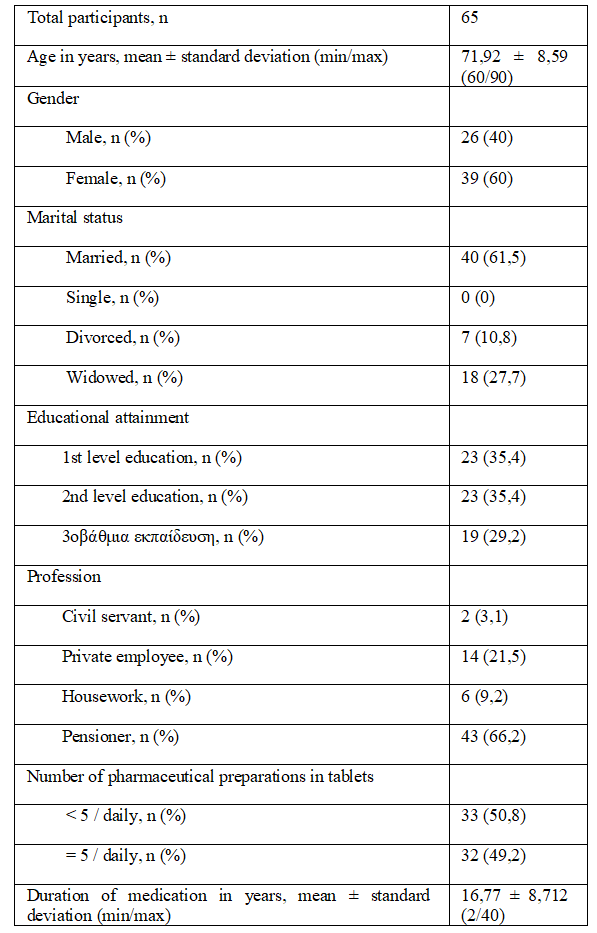
The total sample consists of 65 patients, 60 years of age and older, with chronic diseases who take at least one medicinal tablet daily. All participants completed the requested questions without missing a single one. Specifically, 26 men (40.0%) and 39 women (60.0%) participated, with an average age of 71.92 years ± 8.59, with a minimum age of 60 years and a maximum of 90 years. Forty patients (61.5%) were married, none single, 7 (10.8%) divorced and 18 (27.7) widowed. In addition, the majority of patients had primary education, 23 people and secondary education, 23 people, (35.4% and 35.4% respectively) and 29.2% (19 patients) had university education. Forty-three patients (66.2%) were retired, 14 patients (21.5%) were private employees, 6 (9.2%) were engaged in domestic work, and only 2 patients (3.1%) were civil servants. The mean duration of medication was 16.77 ± 8.71 years with 33 patients (50.8%) taking <5 tablets per day and 32 patients (49.2%) taking 5 tablets or more per day. The above results are presented in Table 1.
Table 1. Frequencies, percentages, mean values, standard deviations and min/max variables of the total sample
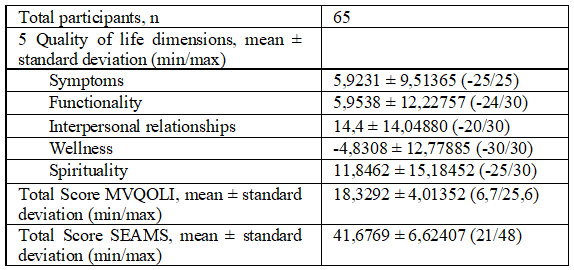
Regarding the results and variables of the questionnaires, the following results were obtained. The result of the total quality of life (Total Score MVQOLI) was formed with a mean value of 18.3292 and a standard deviation of ± 4.01352, a minimum value of 6.7 and a maximum value of 25.6. Regarding the five dimensions of quality of life, symptoms, functionality, interpersonal relationships, well-being and spirituality, the mean values and standard deviations were as follows: 5.9231 ± 9.51365, 5.9538 ± 12.22757, 14.4 ± 14 .04880, -4.8308 ± 12.77885 and 11.8462 ± 15.18452 respectively. The overall result of the compliance questionnaire was formed with a mean value of 41.6769 and a standard deviation of ± 6.62407, a minimum value of 21 and a maximum of 48. The above results are presented in Table 2.
Table 2. Mean values, standard deviations and min/max variables of the questionnaires of the total sample
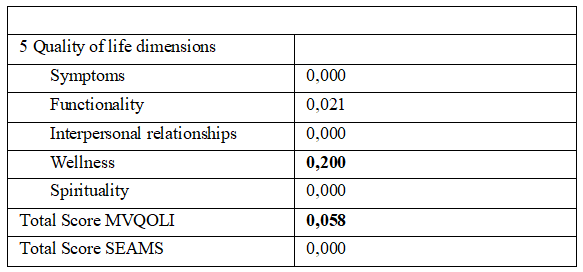
A p-value greater than 0.05 was considered to show normality in the sample under consideration, while values equal to or less than 0.05 did not show normality. Also, p-value equal to or less than 0.05 indicates statistical significance. A Kolmogorov-Smirnov test was then performed to test whether the values of the main variables of the questionnaires (Total Score MVQOLI, Total Score SEAMS and the five dimensions of quality of life) in the total sample fell into a normal distribution. From the analysis it was observed that well-being and the result of the total quality of life (Total Score MVQOLI) show normality with p-values of 0.20 and 0.058 respectively, while the remaining variables under consideration (Total Score SEAMS, symptoms, functioning, interpersonal relationships, spirituality) do not show normality with p-values less than 0.05. It should be noted that the finding of normality or not was an important step for the further statistical analysis as variables that fall into normality follow parametric tests to find correlations with other variables while variables that do not fall into normality follow non-parametric tests in the subsequent statistical analysis. The above results are presented in Table 3.
Table 3. Kolmogorov-Smirnov regularity check, p-value
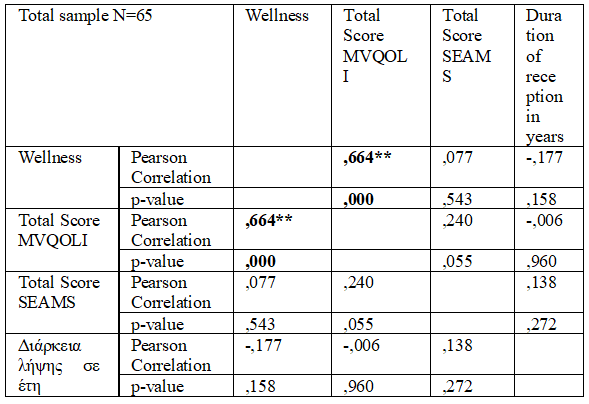
To correlate the variables, which fall into a normal distribution (Total Score MVQOLI and well-being), with other continuous numerical variables (Total Score SEAMS, age and duration of medication in years) to highlight statistically significant results, i.e., p-value equal to or less than 0.05, followed by parametric tests with Pearson's coefficient. The statistical analysis of the total sample showed a strong positive statistically significant correlation between well-being and overall quality of life, with a coefficient of 0.664. No statistically significant results emerged from the correlations of the remaining continuous numerical variables. All of the above are presented in Table 4.
Table 4. Parametric Pearson Correlation of Ordinal Variables with Continuous Numerical Variables in the Total Sample
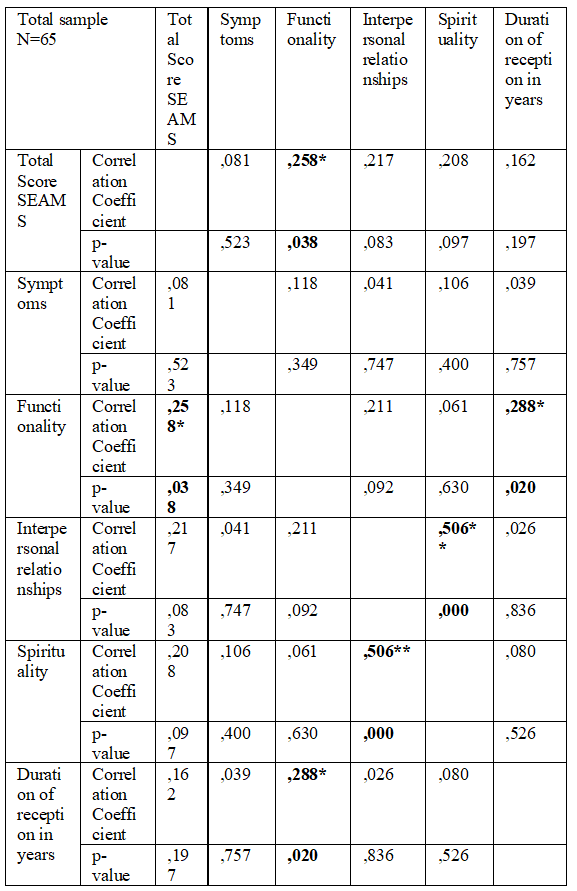
To correlate the variables, which do not fall into a normal distribution (Total Score SEAMS, symptoms, functioning, interpersonal relationships, spirituality), with other continuous numerical variables (age and duration of taking pharmaceuticals in years) to highlight statistically significant results, i.e., p-value equal to or less than 0.05, followed by non-parametric tests with Spearman's rho coefficient. From the statistical analysis of the total sample, a positive statistically significant correlation emerged between functionality and compliance and duration of taking medication, with coefficients of 0.258 and 0.288 respectively. Also, a strong positive statistically significant correlation emerged between spirituality and interpersonal relationships with a coefficient of 0.506. No statistically significant results emerged from the correlations of the remaining continuous numerical variables. All of the above are presented in Table 5.
Table 5. Nonparametric correlation according to Spearman's rho
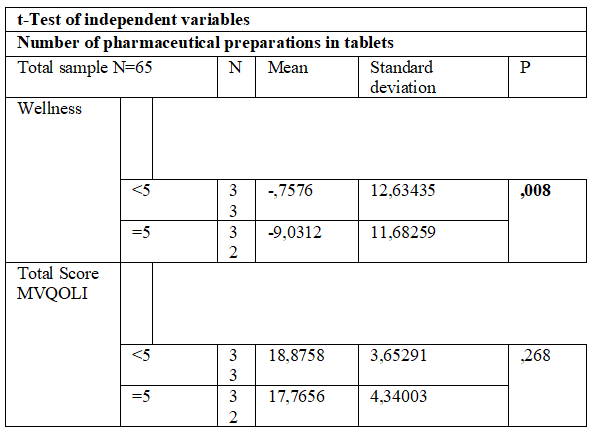
For the relation of the variables, which fall into a normal distribution (Total Score MVQOLI and well-being) with one categorical variable (number of pharmaceutical preparations per day, <5/≥5) to highlight statistically significant results, i.e., a p-value equal to or less than 0.05, followed by t-test of independent variables. The statistical analysis of the total sample revealed that patients who take 5 or more medicinal tablets with a mean value of -9.0312 and a standard deviation of 11.68259 show a lower level of well-being, than patients who take less than 5 medicinal preparations per day, with a mean value of -0.7576 and standard deviation 12.63435. All of the above are presented in Table 6.
Table 6. Parametric Correlation of Ordinal Variables with Intersubjective Categorical (Gender and Number of Pharmaceuticals in Tablets) Variables in the Total Sample
For the relation of the variables, which do not fall into a normal distribution (Total Score SEAMS, symptoms, functionality, interpersonal relationships, spirituality), with intersubjective categorical variable (quantity of pharmaceutical preparations per day, <5/≥5) to highlight statistically significant results, i.e., p-value equal to or less than 0.05, followed by Mann-Whitney t-test of independent variables. From the statistical analysis of the total sample, no statistically significant results emerged.
Discussion
From the analysis of the data of the present investigation, no statistically significant correlation emerged between medication adherence and overall quality of life (p-value 0.055). A total of 65 patients, aged 60 and over, with chronic diseases took part in the research. The majority of them were women (60%) and the rest were men, with an average age of 71.92 years. From the sociodemographic data it emerged that 40 patients were married, 18 widowed and only 7 divorced. As for the educational level, the same ratio of primary and secondary education emerged (23 people each), 19 people with higher education, while 43 people were retired, 6 employed in the household and the rest public or private employees. Also, the factor of polypharmacy, as defined by 5 pharmaceutical tablets or more, was put to study (7,17). The total scores of the two different questionnaires completed by the 65 patients were then calculated, without any loss. The mean value of the total score of the MVQOLI questionnaire was calculated as 18.3292 with a maximum of 25.6, while the scores of the five dimensions of quality of life were calculated separately. The mean value of the compliance questionnaire score was 41.6769 with a maximum of 48.
In addition, for the analysis of well-being, a statistically significant difference (p-value 0.008) was found with the number of different medicinal tablets received by the patients, a situation that is also confirmed by the review of recent literature (25,26). In particular, the more drugs (≥5) patients take daily, the more their level of well-being is burdened, with the difference in the mean value of patients taking less than 5 tablets (-0.7576) being large compared to the group of patients taking equal or more than 5 tablets (-9.0312). Patient functionality appeared to be positively affected by patient adherence to treatment with the result being statistically significant (p-value 0.038). As long as patients are functional in their daily lives, maintaining their personal, social and psychological autonomy is positively affected and adherence to treatment and vice versa (27).
A statistically significant positive correlation was also seen between functionality and duration of medication in years. This result can be interpreted that as the length of years receiving the appropriate medication increases and the intake is consistent, the patients' functionality is maintained and increased as a consequence of good adherence to treatment (28,29).
Some limitations of the present research were that the sample under consideration was a convenience and the number of patients was limited. Questionnaires based on self-report or patient recall data were used, so some information may be biased.
Chronic disease management requires long-term treatment, which includes lifelong drug therapy and lifestyle adjustments. Although clinical outcomes can provide a clear picture of the level of disease control, the ultimate goal of health care delivery should be to improve the patient's overall quality of life, ensuring functionality, autonomy, physical and psychological wellness, to the extent that this is possible. Chronic diseases can have a significant impact on key dimensions of patient well-being, and good adherence to the treatment plan is imperative. Non-adherence to medication is a major contributor to morbidity, mortality and wasted resources in health systems worldwide. Thus, while clinicians tend to talk to their patients about the improvements in clinical outcome associated with taking medications correctly, a greater focus on patient-centered benefits would likely be a more effective strategy for promoting medication adherence. In the context of pharmaceutical care, it appears to be vital to design and use interventions to enhance medication adherence in order to increase available resources and improve the overall quality of life of patients with chronic diseases. To this end, the adoption of patient-centered and individualized interventions and the creation of an excellent collaboration between health professionals and patients, combined with the pursuit of systematic follow-up, are essential to promote both medication adherence and overall quality of life (30,31).